THIS ARTICLE IS MORE THAN FIVE YEARS OLD
This article is more than five years old. Autism research — and science in general — is constantly evolving, so older articles may contain information or theories that have been reevaluated since their original publication date.


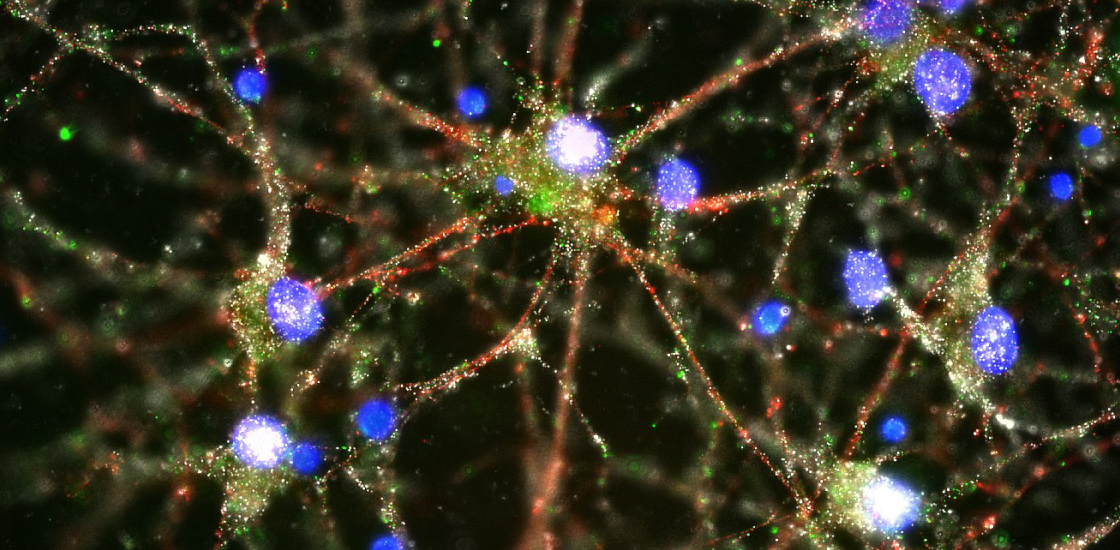
During the first few years of life, the neurons in a child’s brain form billions of connections, or synapses. The brain then proceeds to eliminate some. From toddlerhood until early adulthood, it winnows away unused and redundant links — a process called pruning.
In many cases, an immune molecule called ‘complement’ tags these excess synapses. This molecule serves as an ‘eat me’ signal for immune cells in the brain called microglia, which then gobble up the tagged synapses.
The pruning process may be faulty in the brains of people with autism. This theory is based on evidence that the brains of some children with the condition contain many more synapses than those of controls. In some cases, the brain is overrun with microglia or harbors hyperactive microglia.
Pruning may also go awry in schizophrenia, a condition that shares genetic roots with autism as well as some features, such as difficulties with social interactions and language. But a new study has found that the pruning problems in schizophrenia appear to be the opposite of those in autism: Genetic variants linked to schizophrenia may result in too much pruning rather than too little^1.
We asked the study’s investigators, Steve McCarroll, associate professor of genetics at Harvard University, and Beth Stevens, assistant professor of neurology at Harvard, what these schizophrenia findings might mean for autism research.
Spectrum: What was the goal of your study?
Steve McCarroll: A big mystery in human genetics for seven years was: Why does schizophrenia associate so strongly with common genetic variants in a chromosomal region called the major histocompatibility complex (MHC)? This part of the human genome contains genes important for immune function. Our study was an effort to answer that long-standing question.
Our analyses of the region led us to the complement component 4 (C4) gene. We found that C4 harbors an unconventional form of genetic variation that had not been accounted for in earlier genetic studies. And we were aware of Beth Stevens’ work on complement proteins shaping the wiring of brain circuits. So C4 was a biological candidate as well as a genetic one.
S: When you started your study, what was known about C4?
Beth Stevens: C4 was already known to play a role in the immune system. The protein contributes to the deposition of a related immune molecule, called C3, on pathogens and debris. C3 is an ‘eat me’ signal that’s detected by immune cells, which engulf and destroy any substances labeled with it. But little was known about C4’s function in the brain.
S: Based on your study, how do you think the variants in C4 might lead to schizophrenia?
SM: The MHC region contains two C4 genes, C4A and C4B. What we learned from our work was that different variants in these genes cause them to be expressed at different levels in different people’s brains. We found that the more a variant increases the expression of C4A, the more strongly that variant associates with schizophrenia.
BS: We also found that mice that lack the C4 gene have more synapses than control mice do. Our hypothesis is that too much C4A expression could lead to hyperactivation of the complement cascade during development. And then that could lead to excess pruning of synapses and the altered circuitry found in people with schizophrenia. We’re working together to test that hypothesis.
S: Is there any genetic evidence from people with autism that implicates C4 or genes like it?
SM: No. Genetics studies in autism have tended to focus on rare mutations that have sledgehammer effects on brain development. The genetic variation in C4 that we linked to schizophrenia is different. It is part of the reservoir of common, inherited genetic variation that is present all around us. And it is a quantitative risk factor, meaning that it’s present in a large fraction of cases, but is not a deterministic ‘cause’ in anyone. We think of C4 as moving a threshold, but other genetic and environmental factors determine whether that threshold is crossed. To find genetic influences like that, one has to do genetic studies in large numbers of people.
Our study involved analysis of genetic data from more than 64,000 people. That was what it took to be able to attach a specific level of schizophrenia risk to each version of the gene. Genetics studies have not yet been done in autism on that scale, and so, unfortunately, it is too early to say whether there are genetic effects like this shaping autism risk.
S: What are the next steps for autism researchers?
SM: Well, certainly, larger genetics studies should make it possible to appreciate the influences of common as well as rare variants on autism.
BS: I think another thing that would be good to know is whether there are defects in synaptic pruning in animal models of autism in parts of the brain in which pruning has been well established.
Our work also raises the idea that aberrant pruning by microglia could be something that might be relevant to both schizophrenia and autism. But we still have a lot that we don’t understand about that. For instance, are microglia truly abnormal early in development in autism, or is that just a reaction to some other underlying neuronal or circuit problems? Trying to design experiments and come up with the best models to try to tease that out is important.
By joining the discussion, you agree to our privacy policy.