THIS ARTICLE IS MORE THAN FIVE YEARS OLD
This article is more than five years old. Autism research — and science in general — is constantly evolving, so older articles may contain information or theories that have been reevaluated since their original publication date.
Mice missing the Rett syndrome gene, MeCP2, from neurons that dampen brain activity have hallmark signs of the disorder, such as social abnormalities, repetitive behaviors and poor motor coordination. A new study suggests that most of these symptoms stem from MeCP2 loss in just two types of these so-called ‘inhibitory’ neurons.
The findings, published 18 November in Neuron, begin to reveal the cell types underlying specific sets of Rett-related symptoms1. Children with the condition have intellectual disability, poor coordination, seizures, breathing difficulties and, often, autism.
In 2010, Huda Zoghbi and her colleagues at Baylor College of Medicine in Houston, Texas, showed that mice lacking MeCP2 in inhibitory neurons that send signals through the chemical messenger gamma-aminobutyric acid (GABA) show a range of Rett-like features. That finding pointed to a large role for GABA in the syndrome2.
In the new study, Zoghbi’s team further defined that role by creating two additional mouse models, each of which lacks MeCP2 in just one type of GABA neuron. One of the models has problems with cognition, motor skills and social behavior, whereas the other shows signs of repetitive behaviors and seizures. Together, the two models recapitulate most of the Rett-like features seen in the 2010 study.
“Surprisingly, the two mice developed very different, non-overlapping behavioral deficits,” says Zoghbi, director of the Jan and Dan Duncan Neurological Research Institute at Texas Children’s Hospital in Houston.
The findings may aid the development of treatments, says Darren Goffin, lecturer in neuroscience at the University of York in the U.K., who was not involved in the study. “You may be able to perhaps one day develop ways to target and restore the function of those neurons, and thereby treat certain symptoms of the disorder,” he says.
Singled out:
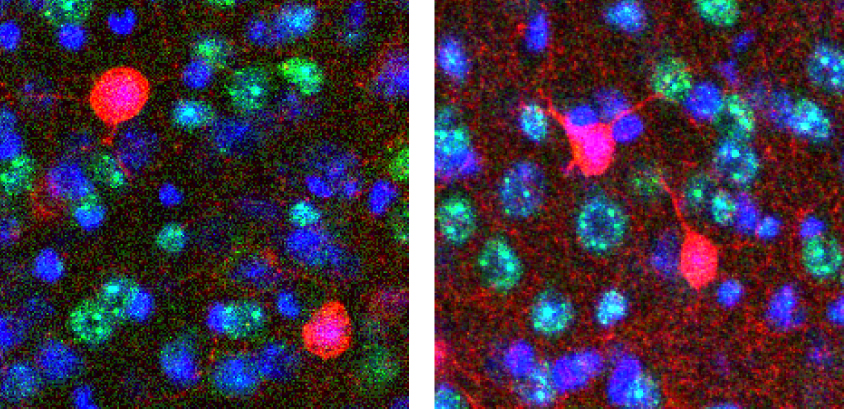
Zoghbi and her team engineered two strains of mice that lack MeCP2 in inhibitory neurons. One strain lacks the gene in neurons that express the molecular marker parvalbumin, the other in neurons that produce a marker called somatostatin. Together, these subtypes constitute the majority of inhibitory neurons in the brain.
By 6 weeks of age, mice lacking MeCP2 in parvalbumin neurons begin to lose motor skills. They have trouble walking on a narrow beam and fall off a rotating rod sooner than controls do.
By 8 weeks of age, the mice do not startle as easily as controls in response to a loud noise, suggesting that they have sensory deficits. At 14 weeks, they spend more time than controls do interacting with an unfamiliar mouse, hinting at abnormalities in their social interactions. They also have trouble learning to associate a certain tone with a painful foot shock, indicating problems with learning and memory.
By contrast, mice that lack MeCP2 in somatostatin neurons perform normally on tests of motor, social and cognitive abilities. However, by 12 weeks of age, they begin to have seizures. They also show repetitive behaviors: When placed on a surface with 16 holes, they tend to poke their nose into the same hole multiple times.
The only unusual feature the two animal models share is premature death. More than half of the animals in each group die by 35 weeks of age. Boys who lack MeCP2 also tend to die in infancy or before birth.
“Both types of mice died prematurely, arguing that there are several key circuits that, if compromised, can lead to this,” Zoghbi says.
Key circuits:
The findings underscore the important role of GABA signals in Rett syndrome, says Zhong-wei Zhang, associate professor at The Jackson Laboratory in Bar Harbor, Maine, who was not involved in the study. “And by doing cell-type specific deletions, they show that the circuits associated with these particular types of cells are likely to be really important for the disease process,” he says.
Yet neurons that communicate using GABA don’t function in isolation. “I think other types of cells are probably important as well,” Zhang says.
For instance, previous efforts have revealed the importance of medulla and spinal cord neurons in breathing problems in Rett syndrome3. They have also shown that excitatory neurons that use the chemical messenger glutamate play a role in seizures4.
Other types of inhibitory neurons may also contribute to symptoms. The new mouse models fail to capture a few features of mice that lack MeCP2 in every GABA neuron. For example, the mice in this study are neither overweight nor lethargic — features of the earlier mouse model.
An important next step is to figure out how the loss of MeCP2 from specific neuron subtypes affects the function of key neural circuits, Zhang says. “Do the cells release less neurotransmitter, or form synapses differently, or receive different connections?”
Because parvalbumin and somatostatin neurons are scattered throughout the brain, scientists also need to figure out whether certain brain areas are particularly susceptible to MeCP2-induced abnormalities, Zhang says. “Which circuit plays a bigger role in certain types of behavior still needs to be studied carefully.”
By joining the discussion, you agree to our privacy policy.