THIS ARTICLE IS MORE THAN FIVE YEARS OLD
This article is more than five years old. Autism research — and science in general — is constantly evolving, so older articles may contain information or theories that have been reevaluated since their original publication date.
A drug that curbs the expression of MeCP2, a gene duplicated in people with a certain autism-linked syndrome, normalizes brain function and reverses abnormal behaviors in mice1.
The findings, reported 25 November in Nature, highlight the potential of a highly specific treatment for people with MeCP2 duplication syndrome, which is marked by autism, intellectual disability, anxiety and seizures. The drug consists of short strands of ‘antisense’ RNA that block MeCP2 expression. A similar antisense drug for children with spinal muscular atrophy is in late-stage trials.
“I’m really super excited about this, because we’re reversing symptoms in animals that have been sick for months,” says lead researcher Huda Zoghbi, director of the Jan and Dan Duncan Neurological Research Institute at Texas Children’s Hospital in Houston.
Having an extra copy of MeCP2 leads to an excess of the protein, which binds to DNA and regulates the expression of thousands of genes. Mutations that decrease the amount of functional MeCP2 protein lead to Rett syndrome, which is, curiously, characterized by symptoms similar to those of MeCP2 duplication syndrome.
In 2007, researchers in the U.K. reversed symptoms in a mouse model of Rett syndrome by restoring MeCP2 expression2. The new study shows that eliminating excess MeCP2 has a similar effect in mice with an extra copy of the gene.
“This is extremely exciting, because it proves that the symptoms are reversible,” says Lucas Pozzo-Miller, professor of neurobiology at the University of Alabama at Birmingham, who was not involved in the study. “There is a very clear and straightforward path from these data to test if this [drug] can have efficacy in kids.”
Genetic proof:
To test the effects of lowering MeCP2 expression in mice, Zoghbi’s team first engineered male mice to carry a copy of the human MeCP2 gene along with their mouse version. (Because MeCP2 resides on the X chromosome, males usually have only one copy of the gene.) A molecular tweak to the mouse gene allowed the researchers to turn it off by injecting the mice with a compound called tamoxifen.
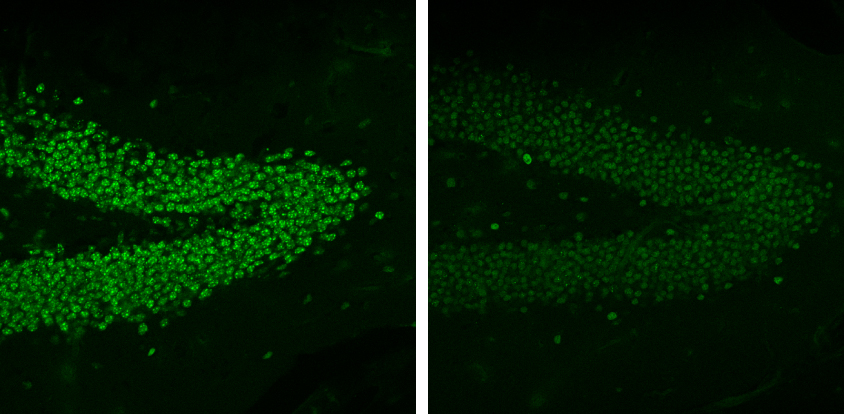
Mice with the duplicated gene are anxious: In an open arena, they spend less time exploring and tend to stick near the perimeter rather than cross through the center of the space as controls do. They also show problems on a test of motor skills, and show little interest in other mice, hinting at social deficits.
When the researchers measured neural activity in brain tissue from the mice, they found abnormal signaling in the hippocampus — a region involved in learning and memory. The expression patterns of genes regulated by MeCP2 also differ from those of control mice.
The researchers turned off the mouse copy of MeCP2 in adult mice, aged 8 to 9 weeks, by injecting them with tamoxifen three times a week for four weeks. Within two weeks after the end of treatment, the mice showed almost no expression of mouse MeCP2 and normal levels of the human copy. They were also indistinguishable from controls on tests of anxiety, motor abilities and social behaviors, and their brain signaling looked normal.
Drug test:
With these results in hand, the researchers partnered with the California-based Isis Pharmaceuticals, one of the firms testing the spinal muscular atrophy treatment, to develop an antisense drug that would block the expression of human MeCP2. They delivered the drug continuously for four weeks through a tiny implantable pump in the mouse brain.
The treatment almost completely blocked the expression of the human gene in the mouse brain. The mice still had normal levels of the mouse version of the gene. The effect persisted for four weeks after the treatment ended.
By six weeks after the treatment ended, the mice no longer showed motor abnormalities, social deficits or signs of anxiety. They also showed normal levels of expression of MeCP2-regulated genes in the brain.
The researchers then tested the treatment in older mice, at 25 to 35 weeks of age. At this age, mice with a duplicated copy of MeCP2 show erratic electrical activity in their brains and have seizures. Injecting the drug into these mice normalized their brain waves and prevented seizures.
“For me, that’s the most exciting part,” Zoghbi says. “The animals at that age are pretty sick.” Because seizures can be debilitating, the possibility of preventing them is encouraging, she says.
Balancing act:
Optimizing the treatment for people may be tricky: Because the drug targets the human copy of the gene, in people it would target all copies of the gene, raising the risk of side effects. Suppressing production of MeCP2 too much could induce Rett-like symptoms, says Stuart Cobb, lecturer in neuroscience at the University of Glasgow in the U.K., who was not involved in the study.
To address this concern, Zoghbi and her colleagues have calibrated the drug dose in blood cells from people with MeCP2 duplication syndrome. So far, they have been able to partially block MeCP2 expression, lowering protein levels to normal. They plan to repeat this dosing test in mice engineered to carry two copies of the human version of MeCP2 and no mouse version, to mimic the situation in people.
Delivery of the drug is not trivial, either. Because the drug cannot pass from the bloodstream into the brain, children would need repeated injections into their cerebrospinal fluid.
Still, the approach is extremely promising, says Kevin Foust, assistant professor of neuroscience at The Ohio State University in Columbus, who was not involved in the study. Foust leads a team that is developing an alternative strategy to lower MeCP2 levels, involving gene therapy. He says his team has unpublished evidence that his strategy has effects similar to those of the antisense approach.
“If you go to the master regulator — the actual root of the problem — as this group has effectively done, then you can change lots of things all at once,” Foust says. “Now, the mission becomes getting this to people.”
By joining the discussion, you agree to our privacy policy.