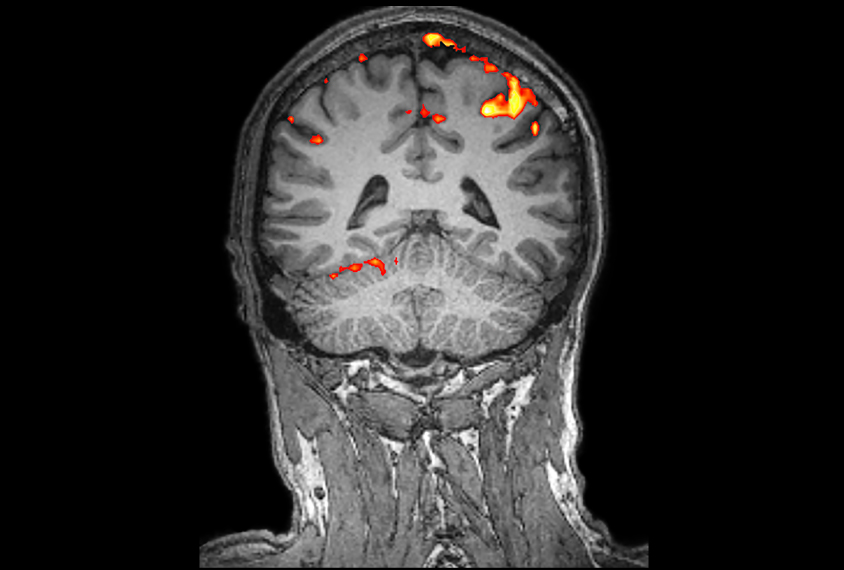
Kul Bhatia / Science Source
THIS ARTICLE IS MORE THAN FIVE YEARS OLD
This article is more than five years old. Autism research — and science in general — is constantly evolving, so older articles may contain information or theories that have been reevaluated since their original publication date.
A new tool spots shared patterns of brain connectivity among people who have autism, schizophrenia or major depressive disorder. Researchers presented the unpublished results today at the 2016 Society for Neuroscience annual meeting in San Diego.
The researchers used a machine-learning algorithm to analyze brain scans from roughly 500 individuals with one of the three conditions or a fourth condition, bipolar disorder.
Their findings reveal two distinct subgroups of people with autism: one with patterns of brain connectivity similar to those seen in schizophrenia, and another with patterns seen in people with either schizophrenia or major depressive disorder.
The results may steer clinicians toward personalized treatments that bridge the traditional diagnostic boundaries — as defined in the “Diagnostic and Statistical Manual of Mental Disorders” (DSM) — between these conditions.
“Hopefully, these biotypes will inform more robust treatments for these individuals, regardless of their standard DSM categories,” says lead researcher Giuseppe Lisi, a postdoctoral researcher at the Advanced Telecommunications Research Institute International in Kyoto, Japan.
Scientists have used various tactics to tease out the underlying similarities between autism and related conditions. Most studies have focused on shared genetic roots or similar behavioral features. Lisi’s team focused on neurological features, which are shaped by genetics and help drive behavior.
Missed connection:
The researchers examined functional magnetic resonance imaging scans from 145 adults with autism, 98 with schizophrenia, 50 with obsessive-compulsive disorder and 200 with major depressive disorder. The scans, collected from multiple Japanese hospitals, were captured while participants were awake and resting.
In an April study in Nature Communications, the researchers used a version of the machine-learning approach to analyze brain connections in people with autism, schizophrenia or attention deficit hyperactivity disorder1. Their analysis revealed that autism most closely resembles schizophrenia.
In the new study, the researchers created several new iterations of the method so that they could measure the resemblance of every condition to each of the other three — except this time, they swapped out attention deficit hyperactivity disorder for bipolar disorder or obsessive-compulsive disorder. They also looked at combinations of the groups.
Their analysis revealed overlapping patterns of brain activity that blur the distinction between diagnostic groups.
The researchers identified four distinct patterns, or ‘biotypes,’ of connectivity among the conditions.
“These biotypes show us information that we wouldn’t have known if we relied on standard DSM categories. Now we can look at the issue of mental disorders from different points of view,” Lisi says.
His group is evaluating individuals in each group for behaviors that might track with their shared connectivity patterns.
For more reports from the 2016 Society for Neuroscience annual meeting, please click here.
By joining the discussion, you agree to our privacy policy.