THIS ARTICLE IS MORE THAN FIVE YEARS OLD
This article is more than five years old. Autism research — and science in general — is constantly evolving, so older articles may contain information or theories that have been reevaluated since their original publication date.
Mutations in stretches of the genome that are specific to humans may play a role in autism, according to a study published 6 October in Cell1. Most of these so-called ‘human accelerated regions’ (HARs) do not code for proteins, but may control genes required for brain development.
Some experts are skeptical of this theory, saying the findings apply to only one type of family included in the study — those in which the parents are closely related to each other.
The study is one of many in the past year suggesting that regions of the genome that do not code for proteins contribute to autism risk.
“Noncoding mutations are probably going to be increasingly implicated as a cause of autism,” says lead investigator Christopher Walsh, professor of neurology at Harvard University.
The study suggests a new focus for scientists scanning whole genomes for autism risk.
“This study shows that one place to really shine the light on would be these human accelerated regions,” says Nadav Ahituv, professor of bioengineering and therapeutic sciences at the University of California, San Francisco, who was not involved in the study.
Hardy HARs:
The sequences of HARs are similar across mammals. But the regions changed rapidly after humans diverged from chimpanzees, suggesting that they were involved in the evolution of distinctly human features. Walsh and his colleagues reasoned that if HARs underlie humans’ complex social and cognitive abilities, mutations in the regions might contribute to autism.
The researchers analyzed mutations in 2,100 children with autism and their unaffected siblings from ‘simplex’ families, in which only one child has autism.
They looked for large duplications or deletions in DNA — known as copy number variations (CNVs) — that include HARs. They found that spontaneous, or non-inherited, CNVs occur 6.5 times more often in people with autism than in their siblings.
However, Walsh and others say that all but two of these CNVs also overlap with parts of the genome that code for proteins. This makes it difficult to parse how much the HARs alone contribute to autism risk.
“The data do not really support the claim that deletions or duplications of HARs contribute to autism,” says Jonathan Sebat, chief of the Beyster Center for Molecular Genomics of Neuropsychiatric Diseases at the University of California, San Diego, who was not involved in the study. “It’s very possible that the HARs are just collateral damage.”
Telling trio:
Walsh and his colleagues then looked at HAR mutations in a set of consanguineous families, in which the parents are closely related to each other. They combed the genomes of 218 people with autism in these families and 177 unaffected parents and siblings for rare, single-letter changes in HARs. Children in these families have an increased chance of inheriting the same mutation from each parent, meaning the mutation affects both copies of the chromosome.
The researchers found that changes in both copies of a given HAR occur 43 percent more often in people with autism than in their unaffected relatives. That number rose to 76 percent when they restricted their search to HARs that regulate genes expressed in the brain.
Overall, mutations in HARs underlie up to 5 percent of autism cases in the consanguineous families in the study, the researchers say.
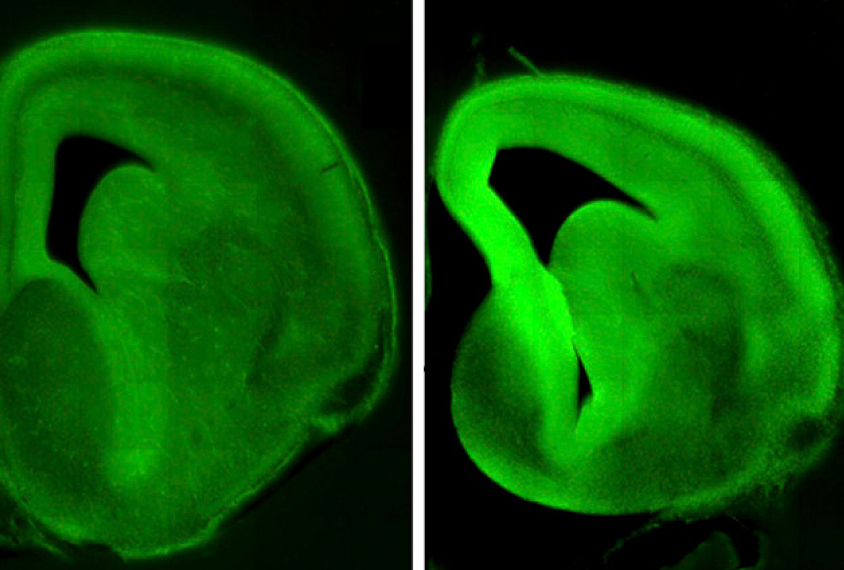
The team characterized three of the mutations that occur next to or within genes involved in brain development. One of these genes, CUX1, regulates the number of neuronal junctions, or synapses. Three people with autism from two unrelated families have the same mutation in a HAR near this gene.
Two brothers with autism carry a mutation in a HAR near PTBP2, a gene previously linked to autism and intellectual disability. And two people with autism from unrelated families have different mutations in a HAR near GPC4, a gene required for the formation of synapses.
Overall, the findings provide compelling evidence that mutations in HARs contribute to autism risk in consanguineous families, but their importance relative to other mutations is uncertain, says Stephan Sanders, assistant professor of psychiatry at the University of California, San Francisco, who was not involved in the study.
It is also unclear whether mutations in HARs are important in non-consanguineous families. Sanders says he has not found mutations in HARs in 500 people with autism from simplex families. “Still, we might need a larger number of families to see it,” he says.
By joining the discussion, you agree to our privacy policy.