THIS ARTICLE IS MORE THAN FIVE YEARS OLD
This article is more than five years old. Autism research — and science in general — is constantly evolving, so older articles may contain information or theories that have been reevaluated since their original publication date.
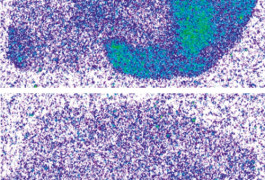
Musical chairs: CTEP, a drug target for fragile X syndrome that blocks access to a receptor in the brain (bottom), prevents binding of a radioactive compound (green) .
A promising approach to treating fragile X syndrome could benefit people even after the critical window of early brain development, and alleviate core symptoms of autism, according to two studies published this month.
Fragile X syndrome is caused by the loss of a single protein, FMRP, and is characterized by intellectual disability, unusual physical features and hyperactivity. As many as 30 percent of individuals with the syndrome also have autism; however, the underlying biology of fragile X syndrome may be distinct from that of autism.
The first study, published 12 April in Neuron, provides the first published evidence that many symptoms of fragile X syndrome may be reversible after they have developed1.
Although the results were shown only in mice, they suggest that a similar effect might be seen in people with the disorder, researchers say.
“Parents of adult patients have always thought that these kinds of new treatments might be too late for them, but this gives them a lot of hope,” says Randi Hagerman, medical director of the MIND Institute at the University of California, Davis. Hagerman was not involved in the new study, but is conducting clinical trials for fragile X therapeutics.
The study was made possible because of a new compound, dubbed CTEP, that is remarkably stable in mice, allowing researchers to study the effects of long-term drug treatment on the brain and behavior.
Mice that model fragile X syndrome started taking the compound at 4 to 5 weeks of age — the equivalent of adolescence in people — and showed a reversal of many neurobiological and behavioral symptoms after four weeks of treatment, the study found.
The second study, published last week in Science Translational Medicine, suggests that drugs developed to treat fragile X syndrome could also help individuals with other forms of autism2.
The study shows that inbred mouse strains that mimic many of the features of autism are more social and show fewer repetitive behaviors when treated with a compound designed for fragile X syndrome that targets the same pathway as CTEP.
“It’s incredible. It didn’t have to work out like that,” says Mark Bear, Picower professor of neuroscience at the Massachusetts Institute of Technology and lead investigator on the Neuron study. “But I’m very pleased that it did.”
Promising pathway:
Both compounds target a cell-signaling pathway that is activated by a receptor molecule, called mGluR5, and which boosts the synthesis of many of the same proteins that are repressed by FMRP3. The mGluR family of receptors normally binds to glutamate, a chemical messenger that activates signals in the brain.
Most mGluR5 proteins sit on the outside of the signal-receiving ends of neurons, making them easy targets for small-molecule compounds that inhibit their activity. A 2007 study showed that cutting the number of mGLuR5 receptors in half in mice that model fragile X syndrome resolves many of the symptoms of the disorder4.
Seaside Therapeutics, a biotechnology company co-founded by Bear, and pharmaceutical giants Roche and Novartis have each developed therapeutic compounds targeting the mGluR5 pathway.
Roche, which co-led the Neuron study, is developing RG7090, an inhibitor of mGluR5 that is currently in clinical trials. CTEP is a mouse version of RG7090. RG7090 has a significantly shorter half-life in rodents compared with people, which makes studying the effects of chronic treatment challenging. By contrast, one dose of CTEP, which can be taken orally, deactivates most mGLuR5 receptors in the brain for about 48 hours.
A single dose of CTEP is enough to reverse the same features of fragile X syndrome — such as an overproduction of proteins in the brain and susceptibility to seizures — as those treated by previous mGLuR5 inhibitors. It also corrects a process that allows neurons to change the strength of their connections in response to learning.
But it took at least four weeks of continued treatment to see improvements in the behavioral features of the syndrome, including sensory sensitivities and problems with learning and memory.
After a total of 17 weeks of drug treatment, the equivalent of several years in people, CTEP alleviates the hyperactivity seen in fragile X mice. It also reduces the size of their testes, which are abnormally large in fragile X syndrome — a condition called machroorchidism.
“The fact that it reversed so many of the different symptoms, even the machroorchidism, is amazing,” says Hagerman.
Other researchers note that in contrast to the mutant mice, the drug has only marginal effects on the neurobiology and behavior of control mice.
“This is the effect you want,” says Kimberly Huber, associate professor of neuroscience at the University of Texas Southwestern Medical Center in Dallas. “If you’re affecting normal functioning of the brain by blocking mGLuR5, that would not be desirable.”
The study shows that the ‘critical window’ that allows for changes in the brain extends at least into adolescence in mice. Long-term drug treatment actually altered the neurons in the brains of the mice: The high density of dendritic spines — mushroom-like bodies on the signal-receiving branches of neurons — that is a feature of fragile X syndrome returned to control levels after four weeks of treatment.
Social function:
The secondstudy used a different inhibitor of mGLuR5 activity, developed by Pfizer for research purposes, called GRN-529.
This study focused on two inbred strains of mice, which are lines in which both copies of each of their genes are identical. One of these strains, called BTBR, has characteristics that closely mimic the core deficits of autism. For example, BTBR mice show little interest in interacting with other mice, emit fewer ultrasonic vocalizations — cries that are inaudible to the human ear — in response to social cues, and go through long bouts of self-grooming.
The other strain, called C58/J, has a tendency to jump repeatedly — a behavior that may model the repetitive behaviors seen in individuals with autism.
No drug treatments are currently approved to treat the core symptoms of autism, in particular social deficits.
After BTBR mice are treated with a single dose of GRN-529, they groom themselves less frequently during a ten-minute interval than those given a placebo, the study found. This finding is in line with results shown for MPEP, another mGLuR5 inhibitor that has been tested in these mice. GRN-529 treatment also lessens the repetitive jumping seen in the C58/J mice.
Most significantly, BTBR mice treated with the drug are more social than their untreated counterparts, the study found. They are more likely to choose to investigate another mouse in their cage instead of an object and to touch noses with other mice when allowed to freely interact.
An effect on social behavior “seemed extremely optimistic,” says lead investigator Jacqueline Crawley, chief of behavioral neuroscience at the National Institute of Mental Health.
The results suggest that fragile X drugs that target mGluR5 could also treat autism. Researchers at Pfizer are planning to test the compound on mice with some of the genetic mutations associated with autism, including duplications and deletions of genomic regions. And drug companies plan to eventually extend clinical trials for fragile X syndrome drugs to individuals with autism, says Hagerman.
But showing an effect in mice is still a long way from treating people, researchers caution.
“It is not known if the gene mutations that alter behavior in the BTBR mice actually contribute to autism in humans, and the surface resemblance of mouse and human behaviors can be very misleading,” notes Bear.
An advantage of these mouse studies, however, is that they allow researchers to perform experiments that are not easy to do in clinical trials.
Elizabeth Berry-Kravis, professor of pediatrics, biochemistry and neurology at Rush University Medical Center in Chicago, hopes that the fact that some symptoms took as long as 17 weeks to correct in the fragile X mice will encourage drug companies to conduct longer clinical studies.
“I don’t think any of us expect people to just wake up and be better. It’s going to take time. You have to have experience and to learn, even if your brain is in a little bit of a better place to do that learning,” she says.
Crawley also says that she is “cautiously optimistic” that the promising results in the mouse studies could extend to people. “There are many reasons why something might work in mice and not in people, but this is at least a proof of principle that the mGluR5 receptor is a good target to keep looking at for treatments for autism.”
Despite the promise of drugs targeting the mGLuR5 pathway, Bear says that researchers shouldn’t stop looking for another approach. “We shouldn’t now give up. We need to continue to work on targeting other steps in this signaling pathway with the hopes of having more shots on goal,” he says.
By joining the discussion, you agree to our privacy policy.