Spectrum: Autism Research News
Why autism seems to cluster in some immigrant groups
Cultural barriers lead clinicians to misdiagnose or miss children with autism in immigrant communities.

Around 2 p.m. on a perfect summer afternoon in 2014, the clinicians arrived at Maki Gboro’s home in Denver, Colorado, to test his 18-month-old son Baraka for autism. The family had only recently moved to the United States from the Democratic Republic of Congo: Gboro came first, in 2009. His wife Odile Nabunyi arrived in 2013 with their two sons. They later had a third child, but at the time, Baraka was the youngest.
Gboro and Nabunyi sat on a sofa in the living room of their apartment and watched as the women from a community health clinic offered the toddler various objects. The women’s goal was to observe how Baraka would play with the objects — standard protocol for an autism evaluation. But the protocol seemed geared toward a child with a typical American upbringing. There was a pretend birthday cake, but Baraka had not yet been to an American birthday party. They gave him a plastic bag of Cheerios, the popular American breakfast cereal, but a typical breakfast in the Congo — and in Gboro’s household — is cheese, bread and milk, or sometimes porridge. And there was an African interpreter, too, but he spoke an unfamiliar French dialect and gave the boy instructions with words his parents never used. Sometimes, the clinicians spoke directly to Baraka in English, which he didn’t understand at all.
The autism diagnosis that followed left Gboro feeling surprised and uncertain.
“My first reaction was that I didn’t get it,” says Gboro. He had been a physician in the Congo and knew about autism, but had seen few children with the condition before his son was diagnosed. “In our culture, kids are different; some are active, some are quiet … I really didn’t see that coming.” Only after talking with a therapist and another Congolese family with the same diagnosis did he begin to understand more about how to help his son.
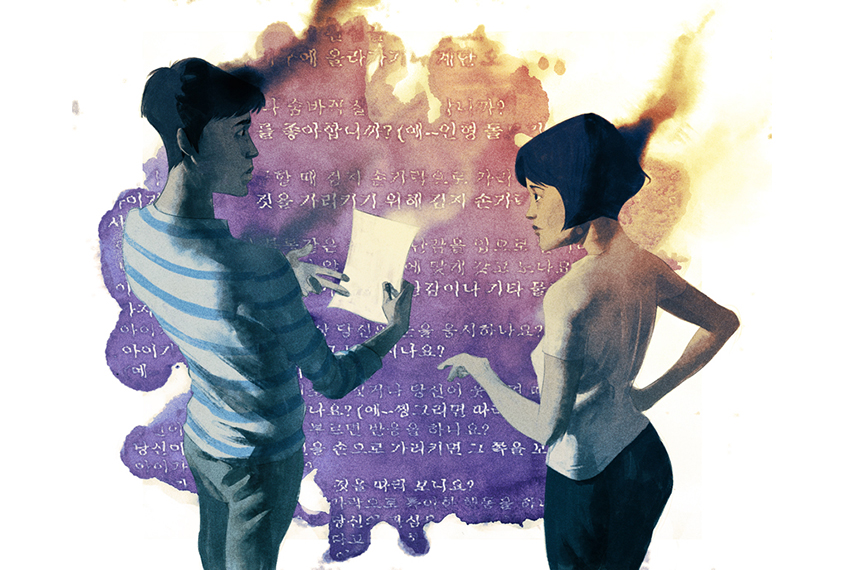
For any family, navigating an autism diagnosis is a long process full of paperwork, questions and decisions. When those conversations happen in a foreign language within an unfamiliar healthcare and educational system, the confusion can escalate — especially among people from cultures like Gboro’s that stigmatize mental illness or have no concept of autism at all.
Those complexities, experts say, make it difficult to interpret the evidence that certain immigrant communities have an unusually high or low prevalence of autism. As some researchers dig into possible explanations, from stress to environmental factors, others say the true issue may be societal: a mix of diagnostic challenges, communication barriers and culture clashes that lead clinicians to misdiagnose or miss children on the spectrum in these communities.
Some teams are trying to develop or assess screening tools tailored for certain ethnic groups in the U.S. and elsewhere — for example, a picture-based tool for use in Sri Lanka — and these efforts may lead to more accurate numbers among different populations. If the figures reveal true differences in prevalence among these communities, they might offer clues about the potential causes of autism. The vast majority of research on autism today, after all, is limited to mostly white and middle-class families. At the very least, getting a better handle on prevalence may help identify populations with the greatest needs for culturally adapted services.
“What’s important is that kids who have autism get identified early and access high-quality treatment,” says Katharine Zuckerman, a pediatrician at Oregon Health and Science University in Portland. “I think we do a pretty poor job of that in this country, especially if you look at the most evidence-based treatments for autism — only a small fraction gets that. And immigration influences the ability to access those things.”

How many?
Gboro had begun to grow concerned about Baraka about eight months before the clinicians arrived at his home. He had not lived with Baraka full-time until the family reunited in Colorado, but as the child settled into his new surroundings, Gboro noticed that his son didn’t speak much. And the boy was hyperactive — he never sat still and he needed to spend a lot of time playing. Gboro asked the family pediatrician if he thought Baraka might have attention deficit hyperactivity disorder. The doctor reassured Gboro the boy seemed fine, but agreed to refer the child for further evaluation.
When the autism diagnosis came, Gboro knew what it meant in his community. Some Congolese people, even those who have been in the U.S. for years, refer to autism as a ‘curse.’ Some are even more fatalistic. “They say, ‘It’s just a disease that God gives you and you cannot do anything about it,’” Gboro says. Social ostracism often follows, isolating families with a child on the spectrum. As a result, he says, many Congolese children on the spectrum are never screened or diagnosed and miss out on early intervention — the only thing known to help. The families also miss out on social support — an outcome Gboro says his family has been able to avoid by being selective about where they go and with whom they spend their time.
Those kinds of problems play out well beyond the Congolese community in the U.S. About one in four children in the U.S. has parents who are immigrants. The official estimate for autism prevalence nationwide, based on educational and medical records, is 1 in 68. But it’s still not clear how accurate those numbers are for any groups. And individual states report wide-ranging numbers — from 1 in 93 in Wisconsin to 1 in 58 in Utah.
Such discrepancies may stem from differences in the surveillance programs or in available services rather than real ups and downs in prevalence. For example, when a state mandates services for people with autism, Zuckerman says, the prevalence of autism in that state goes up. These same issues reverberate through immigrant communities. Most prevalence studies rely on data from doctors or schools that refer children for special services, but those children may never be counted if their immigrant parents are reluctant or unsure about how to ask for help. (The same dynamic might explain research suggesting that racial minorities and children from low-income families are less likely to have an autism diagnosis than children from affluent or white families.)
Researchers have tried to fill those blind spots — with conflicting and provocative results. One clue that migration might play a role in autism came from a 2009 meta-analysis of 40 international studies, which together considered nearly 30 prenatal influences on autism risk. The analysis homed in on some factors that seem to track with an increase in autism risk, including being an oldest child, having a mother with gestational diabetes or being exposed to medications, particularly psychiatric drugs, in utero. Also on the list: having a mother who was born abroad. That link was strong in studies conducted in Scandinavia but just missed statistical significance overall.
A more focused study published in 2012 reviewed data from nearly 5,000 children with autism in Sweden. About one in five had two parents born outside Sweden, many of them from Africa, western Asia and northern Europe. That analysis found higher rates of autism with intellectual disability in the children of parents who had immigrated from specific regions, particularly resource-poor countries. Compared with families that have two Swedish-born parents, the rates of autism with intellectual disability were nearly twice as high among children whose parents were born in sub-Saharan Africa. The risk was also elevated, albeit less so, among children whose parents came from North Africa, Latin America, the Caribbean and South Asia.
Some of the most high-profile research in any immigrant group has focused on the Somali community in Minnesota, where concerns first cropped up about a potential ‘autism cluster’ around 2008. At that time, the Minnesota Department of Health began looking into what seemed like a disproportionately large number of Somali-American children being flagged for special-education programs in city-funded preschools.
Based on data from 2010, the department estimated that 1 in 32 Somali children in Minneapolis had autism. This number is not much different than the estimated 1 in 36 white children with autism in the city. But both rates are considerably higher than those in non-Somali black children (1 in 62) or Hispanic children (1 in 80) in Minneapolis. The findings were widely covered by local and national media. After that, many Somali-American parents stopped vaccinating their children, which then contributed to a measles outbreak in the city this past April through July.
But the study had major limitations, says lead researcher Amy Hewitt, a disability researcher at the University of Minnesota’s Institute on Community Integration in Minneapolis. For one, the sample size in the study was small, with data on just 255 children with autism out of more than 12,000 children in the schools overall. (Of the total population, about 1,000 children are Somali and 31 of those children have autism.) “The study often gets cited as an international fact or a national fact, and it’s not,” Hewitt says. “It also gets reported as if it were about all Somalis.”
Hewitt’s team is working with the Centers for Disease Control and Prevention to analyze more recent data, from 2014. To get bigger numbers and a clearer picture of prevalence, they are assessing rates within a broader region, encompassing Minneapolis and its twin city, St. Paul. They are also looking at a more diverse set of immigrant communities, including Hmong and other Asian and African groups, as well as Native American children. “We know enough to know there’s a whole lot more we need to know,” Hewitt says.
“We’re probably missing the Somali kids with autism who have lower support needs or not as obvious characteristics.” Amy Hewitt
Risky moves:
Physicians from all over the U.S. have reached out to Hewitt to share their speculations on why autism rates might be elevated among Somali families. None of those theories — from mercury-laden skin-lightening creams to radical shifts in diet among immigrant mothers — have enough evidence to support them. The same holds true for other hypotheses that have been proposed, including the ideas that immigrant mothers may be poorly nourished or had early-life infections.
One emerging theory that is gaining support points to a lack of vitamin D, specifically among Africans who have immigrated to northern latitudes. A study last year of more than half a million Swedish people linked vitamin D deficiency in mothers to an increased risk of autism with intellectual disability in their children. The finding didn’t hold up for children on the milder end of the spectrum. This trend is consistent with previous research, including a small study showing vitamin D deficiency in 19 of 31 immigrant women tested in Sweden. There is some evidence that vitamin D is crucial for brain development.
The 2012 study of Swedish children hints at another possible influence: Among children born to immigrants, autism with intellectual disability is most prevalent among children born within about a year after their mothers moved. This finding suggests that the risk is tied specifically to relocating during pregnancy, says Dheeraj Rai, a psychiatrist at the University of Bristol in the U.K. “This makes us question whether it’s just ethnicity,” Rai says, “or if there’s a role for migration and, particularly, stressful migration.”
The first and only large-scale attempt to dig into the link between migration and autism in the U.S. also implicates a role for maternal stress in autism. That 2014 study was based on data from more than 1.6 million children born in Los Angeles County between 1995 and 2006. It found that children born to women from current or former war zones might be particularly vulnerable to autism. Compared with white children of U.S.-born mothers, autism is 76 percent more common among children of foreign-born black mothers, the researchers found. Autism is also 43 percent more common among children of Vietnam-born mothers and about 25 percent more common among the children of mothers born in Central America, South America or the Philippines. In a 2017 study of children born in Australia, researchers reported that, compared with children of white mothers, children of immigrant families from East Africa were 3.5 times more likely to be diagnosed with autism with intellectual disability. Rates were lower among immigrants from other places.
The Los Angeles researchers offered theories about maternal stress or other causes, but “we have no real proof for any of it,” says lead researcher Beate Ritz, an epidemiologist at the University of California, Los Angeles.
The hypothesis that maternal stress can alter brain development also runs up against multiple studies that have found no relationship between autism and maternal stress, including mourning — even for a child — during or shortly before pregnancy.
There’s another possible explanation for evidence of elevated rates in some groups: The prevalence estimates we have may be wildly wrong — even in the most heavily studied communities.
Hewitt and her colleagues reported in 2013 that 100 percent of Somali-American children diagnosed with autism also have intellectual disability, compared with about a quarter of children who are white, Hispanic or non-Somali black — a number consistent with the nationwide average. Swedish studies have shown a similar pattern. The striking difference suggests that Somali-American children on the milder end of the spectrum are not being counted, Hewitt says.
“I tend to think we’re probably missing the Somali kids with autism who have lower support needs or not as obvious characteristics, and may be passing their symptoms off as English-language learner issues or cultural differences,” she says. “If that’s the case, then the autism rate in the Somali community is way higher.”
There is some evidence that clinicians in Minnesota and elsewhere can be too quick to dismiss classic autism traits as cultural differences. Muhammed was 3 in 2008, when his parents, Bassem Fadlia and Nahla Bakry, learned he might have autism after a routine screening through the school district in Rochester, Minnesota. To follow up, they took Muhammed for an evaluation at the Mayo Clinic, where Fadlia works in information technology. Muhammed had some developmental delays, the clinicians there told his parents, but he didn’t have autism.
Bakry felt relieved but also unsettled. During the toddler’s evaluation, she and Fadlia had observed multiple interactions that were tinged with cultural confusion and made them worry the clinicians were not getting a true read on their son. One question the clinicians asked Muhammed was about shoveling snow. But the family was new to Minnesota and lived in an apartment, so Muhammed had never seen snow shoveled. They showed Muhammed pictures of Disney characters, but he had not seen most of the movies featuring those characters and ignored them. And they asked him to name pictures of animals, including a giraffe, but he sometimes offered the word only in Arabic, the family’s primarily language at home.
The more his parents watched, the more they worried — not so much that Muhammed was missing some of the questions, but that the clinicians were misinterpreting what they saw and giving him passing scores even when he was struggling. After talking with a Lebanese friend who was undergoing autism screening for her child, they eventually sought help from the Minnesota Autism Center, a nonprofit organization. After a full evaluation that took about two days, experts at the center diagnosed Muhammed with autism. The label gave him access to 40 hours of services a week, including speech therapy and a therapy called applied behavior analysis. Now 12, Muhammed has shed his autism diagnosis, achieving what researchers describe as an ‘optimal outcome,’ but retains some problems with attention and with social skills.
Bakry still laments the months it took to get Muhammed the help he needed. “The problem with the Mayo [doctors] and any other physician in the U.S. is that when they see an immigrant having a kid who doesn’t speak or perform how a typical kid would, they would think this is a cultural thing or a language barrier, which was not the case for our son,” she says.
Even when doctors try to be culturally sensitive, many still get it wrong, adds Zuckerman. In a 2013 study of 267 pediatricians in California, she and her colleagues found that less than one-third offered screening for autism in Spanish as recommended by the American Academy of Pediatrics. Only 10 percent offered both Spanish-language autism screening and general developmental screening. The researchers found that doctors had a tougher time assessing autism in Latino children from Spanish-speaking families — and it seems their discomfort makes them more likely to look the other way. “If providers feel uncomfortable about it, they’re more likely to do nothing,” Zuckerman says. “And then diagnosis gets delayed or it just never happens.”
Other studies have found a similar reluctance among doctors: Minority children are often diagnosed later than white children or not at all, and doctors tend to give them passing scores on the autism tests when they shouldn’t. “Providers may have unconscious bias, or because of lack of knowledge, may not recognize how autism presents in diverse kids,” Zuckerman says.
"As people have devised better ways to actually recognize autism in Spanish-speaking folks, the incidence has been going up.” Bruno Anthony
More sensitive screening:
Fixing flawed prevalence rates in immigrant communities calls for screening tools that have been adapted specifically for these families. The translations available so far often miss the cultural mark, however. One meta-analysis of 21 studies assessed the translation of nine widely used screening tools for autism, including the Autism Spectrum Screening Questionnaire, into eight languages, including Arabic. The results exposed a web of complications and altered meanings. Some translations changed questions and, in the process, altered the cutoff scores for diagnosis. For example, a Japanese version of the popular Modified Checklist for Autism in Toddlers (M-CHAT) had to take into account reluctance among parents in Japan to answer “yes” to yes-or-no questions, and a tendency to interpret their child’s lack of interest in other children as mere shyness. In some countries, including Mexico, it is rude to make eye contact or point with your index finger, and questions about both behaviors often show up on screening tools. Parents from various cultures also have different expectations about how their children should behave, research shows. Those differences include when parents think children should reach developmental milestones and how important they think it is to talk to their children.
Given these discrepancies, it’s easy for parents to second-guess themselves, says Rocio Mendez, who moved to the U.S. from Guatemala in 2001. Mendez remembers feeling confused as she worked through the Spanish translation of the M-CHAT in 2009, when her son David was a toddler. One question, in its original form, asked whether parents ever bounced their children on their knees. In Spanish, the question became, “¿A su hijo le gusta jugar al caballito?”
“Literally, if you translate it, it says, ‘Does your child enjoy to play the horse?’” says Mendez. “I was like, ‘My son doesn’t play with a horse at that age.’ With those words, you have to be very careful.”
Developing better tools takes a lot of time and effort, says Bruno Anthony, a child clinical psychologist at the University of Colorado in Denver. Anthony led the meta-analysis of autism screening tools. When he started working with a health center that serves a primarily Latino population in Washington, D.C., his team did an exhaustive search of the literature on Spanish-language screening tools. The one they chose received immediate complaints. One surprise was the response to a question that asked whether the child plays peekaboo. Many of the Latino parents didn’t know what peekaboo was, Anthony says. “They said, ‘You mean, like ‘hide and seek?’”
The team spent two years networking through community organizations and churches to educate people about the value of screening, while also collaborating with providers and talking with families to address their concerns. Before they started the project, less than 10 percent of the families that came to the clinic had their children screened for autism. Afterward, that figure rose to more than 80 percent. The screens flagged 4 percent of those children for further testing, in line with rates elsewhere.
Such intensive efforts are starting to change estimates of prevalence in Latino communities. In early studies from about a decade ago, Latino children were consistently found to have lower-than-average rates of autism. But as rates have increased overall, numbers among Latinos, particularly among those of high socioeconomic status, are also rising. “I think that what’s been happening is that, as people have devised better ways to actually recognize autism in Spanish-speaking folks, the incidence has been going up,” Anthony says.
Even after a child is diagnosed, however, her family may struggle to access services or to communicate with doctors and teachers.
“There are layers and layers of problems in immigrant communities,” says YoungSeh Bae, executive director of the Community Inclusion and Development Alliance, a nonprofit organization that supports Korean-Americans with disabilities. Among the 60,000 or so Korean-American families in Queens, New York, where the organization is based, there may be hundreds of people with disabilities, including autism, she says. Despite extensive research, however, she has found no official prevalence estimates and suspects many of the children lack adequate support.
Bae joined one family on a visit to their son’s school. The teenager has autism and his family had requested a Korean version of his individualized education plan. But the school had used a computer program to translate the document, and no one could understand what it said. “I was born in Korea and couldn’t understand the translation. The characters were all jumbled up,” Bae says.
Faced with similar challenges, Gboro has become passionate about helping immigrants blindsided by diagnoses of autism or other developmental disabilities, just like he was a few years ago. For two years, he worked as a health coordinator at an African community center in Denver, helping refugees navigate the American system. He is studying for his U.S. medical license so he can offer even more direct help.
He says his son Baraka is lucky in many ways: Although it took Gboro and his wife great effort to fill out the piles of papers that accompanied Baraka’s diagnosis, Gboro at least has a medical background. He also had some familiarity with the U.S. healthcare system, including a fellowship in neurodevelopmental disabilities at the University of Colorado. That experience helped him navigate the system and learn quickly, making it easier to find support for his son.
Now almost 5, Baraka is a social and joyful boy who loves gospel music and playing outside. Gboro credits his progress to the therapies he received from a young age. “He still has challenges,” Gboro says. “But he has a lot of strengths. He’s doing really great.”
By joining the discussion, you agree to our privacy policy.