Spectrum: Autism Research News
The controversy over autism’s most common therapy
Applied behavioral analysis is the most widely used therapy for autism, but some people say its drills and routines are cruel, and its aims misguided.

When Lisa Quinones-Fontanez’s son Norrin was diagnosed with autism at age 2, she and her husband did what most parents in their position do — they scrambled to form a plan to help their child.
Ultimately, they followed the experts’ advice. They put Norrin in a school that used applied behavioral analysis, or ABA, the longest-standing and best-established form of therapy for children with autism. They also hired an ABA therapist to direct a home program.
ABA involves as much as 40 hours a week of one-on-one therapy. Certified therapists deliver or oversee the regimen, organized around the child’s individual needs — developing social skills, for instance, and learning to write a name or use the bathroom. The approach breaks desirable behaviors down into steps and rewards the child for completing each step along the way.
ABA was tough on everyone at first, says Quinones-Fontanez: “He would cry sitting at the table during those sessions, hysterically cry. I would have to walk out of the room and turn on the faucet to tune it out because I couldn’t hear him cry.”
But once her son got settled into the routine of it, things improved, she says. Before he began therapy, Norrin did not speak. But within a few weeks, the ABA therapist had Norrin pointing his fingers at letters. Eventually, he learned to write letters, his name and other words on a dry-erase board. He could communicate.
Norrin, now 10, has been receiving 15 hours a week of ABA therapy at home ever since. He is still in an ABA-based school. His therapists help him to practice age-appropriate conversation and social skills, and to memorize his address and his parents’ names and phone numbers.
“I credit ABA with helping him in a way that I could not,” Quinones-Fontanez says. “Especially in those first few years, I don’t even know where we would have been without ABA therapy.”
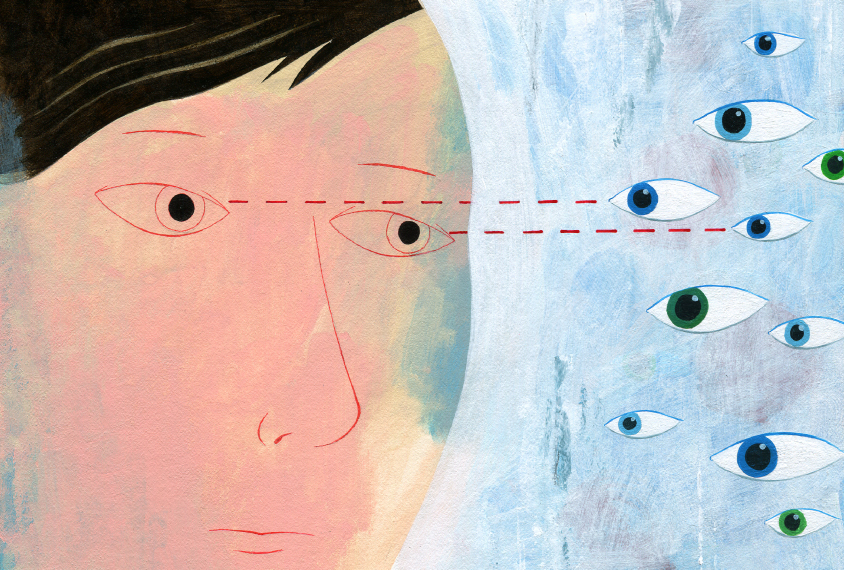
But in recent years, Quinones-Fontanez and parents like her have had cause to question ABA therapy, largely because of a fiercely articulate and vocal community of adults with autism. These advocates, many of them childhood recipients of ABA, say that the therapy is harmful. They contend that ABA is based on a cruel premise — of trying to make people with autism ‘normal,’ a goal articulated in the 1960s by psychologist Ole Ivar Lovaas, who developed ABA for autism. What they advocate for, instead, is acceptance of neurodiversity — the idea that people with autism or, say, attention deficit hyperactivity disorder or Tourette syndrome, should be respected as naturally different rather than abnormal and needing to be fixed.
“ABA has a predatory approach to parents,” says Ari Ne’eman, president of the Autistic Self Advocacy Network and a prominent leader in the neurodiversity movement. The message is that “if you don’t work with an ABA provider, your child has no hope.”
What’s more, the therapy has a corner on the market, says Ne’eman. Most states cover autism therapy, including, often, ABA — perhaps because of its long history. But in California, for example, parents who want to pursue something else must fund it themselves.
These criticisms haven’t made Quinones-Fontanez want to ditch Norrin’s ABA therapy, but they confuse her. She says she can see what the advocates are saying on some level; she does not want her son to become a ‘robot,’ merely repeating socially acceptable phrases on command because they make him seem like everyone else. Sometimes Norrin will approach friendly people on the street and say, “Hello, what’s your name?” as he’s been taught, but not wait around for the answer, because he really doesn’t understand why he’s saying it. “He just knows to do his part,” she says.
The message that ABA might be damaging distresses her. “I’m trying to do the best I can. I would never do anything to hurt my child,” she says. “This is what works for him; I’ve seen it work.”
Whether ABA is helpful or harmful has become a highly contentious topic — such a flashpoint that few people who aren’t already advocates are willing to speak about it publicly. Many who were asked to be interviewed for this article declined, saying they anticipate negative feedback no matter which side they are on. One woman who blogs with her daughter who has autism says she had to shut down comments on a post that was critical of their experience with an intensive ABA program because the volume of comments — many from ABA therapists defending the therapy — was so high. Shannon Des Roches Rosa, co-founder of the influential advocacy group Thinking Person’s Guide to Autism, says that when she posts about ABA on the group’s Facebook page, she must set aside days to moderate comments.
Strong opinions on both sides of the issue abound. Meanwhile, parents like Quinones-Fontanez are caught in the middle. There’s no doubt that everyone wants what is right for these children. But what is that?
A new view:
Before the 1960s, when autism was still poorly understood, some children with the condition were treated with traditional talk therapy. Those who had severe symptoms or also had intellectual disability were mostly relegated to institutions and a grim future.
Against this backdrop, ABA at first seemed miraculous. Early on, Lovaas also relied on a psychotherapeutic approach, but quickly saw its futility and abandoned it. It wasn’t until Lovaas became a student of Sidney Bijou, a behaviorist at the University of Washington in Seattle — who had himself been a student of the legendary experimental psychologist B.F. Skinner — that things began to click.
Skinner had used behavioral methodologies to, for instance, train rats to push a bar that prompted the release of food pellets. Until they mastered that goal, any step they made toward it was rewarded with a pellet. The animals repeated the exercise until they got it right.
Bijou contemplated using similar strategies in people, judging that verbal rewards — saying “good job,” for instance — would serve as adequate motivation. But it was Lovaas who would put this idea into practice.
In 1970, Lovaas launched the Young Autism Project at the University of California, Los Angeles, with the aim of applying behaviorist methods to children with autism. The project established the methods and goals that grew into ABA. Part of the agenda was to make the child as ‘normal’ as possible, by teaching behaviors such as hugging and looking someone in the eye for a sustained period of time — both of which children with autism tend to avoid, making them visibly different.

Lovaas’ other focus was on behaviors that are overtly autism-like. His approach discouraged — often harshly — stimming, a set of repetitive behaviors such as hand-flapping that children with autism use to dispel energy and anxiety. The therapists following Lovaas’ program slapped, shouted at or even gave an electrical shock to a child to dissuade one of these behaviors. The children had to repeat the drills day after day, hour after hour. Videos of these early exercises show therapists holding pieces of food to prompt children to look at them, and then rewarding the children with the morsels of food.
Despite its regimented nature, the therapy looked like a better alternative for parents than the institutionalization their children faced. In Lovaas’ first study on his patients, in 1973, 20 children with severe autism received 14 months of therapy at his institution. During the therapy, the children’s inappropriate behaviors decreased, and appropriate behaviors, such as speech, play and social nonverbal behavior, improved, according to Lovaas’ report. Some children began to spontaneously socialize and use language. Their intelligence quotients (IQs) also improved during treatment.
When he followed up with the children one to four years later, Lovaas found that the children who went home, where their parents could apply the therapy to some degree, did better than those who went to another institution. Although the children who went through ABA didn’t become indistinguishable from their peers as Lovaas had intended, they did appear to benefit.
In 1987, Lovaas reported surprisingly successful results from his treatments. His study included 19 children with autism treated with ABA for more than 40 hours per week — “during most of their waking hours for many years,” he wrote — and a control group of 19 children with autism who received 10 hours or less of ABA.
Nine of the children in the treatment group achieved typical intellectual and educational milestones, such as successful first-grade performance in a public school. Eight passed first grade in classes for those who are language or learning disabled and obtained an average IQ of 70. Two children with IQ scores in the profoundly impaired range moved to a more advanced classroom setting, but remained severely impaired. In comparison, only one child in a control group achieved typical educational and intellectual functioning. A follow-up study six years later found little difference in these outcomes.
The methods promised parents something that no one else had: hope of a ‘normal’ life for their children. Parents began to demand the therapy, and soon it became the default option for families with newly diagnosed autism.
“ABA has a predatory approach to parents.” Ari Ne’eman
A touchstone:
Lovaas’ ABA was formulaic, a one-size-fits-all therapy in which all children for the most part started on the same lesson, no matter what their developmental age.
Michael Powers, director of the Center for Children With Special Needs in Glastonbury, Connecticut, started his career working at a school for children with autism in New Jersey in the 1970s. The therapist would sit on one side of a table, the child on the other. Together, they went through a scripted process to teach a given skill — over and over until the child had mastered it.
“We were doing that because it was the only thing that worked at the time,” Powers says. “The techniques of teaching autistic kids hadn’t evolved enough to branch out yet.” Looking back, he sees flaws, such as requiring children to maintain eye contact for an uncomfortably long period of time. “Five seconds. That was one skill we were trying to establish, as if that was the pivotal skill,” he says. But it was artificial: “The last time I looked someone in the eye for five consecutive seconds, I proposed.”
Doubts grew about how useful these skills were in the real world — whether children could transfer what they’d learned with a therapist to a natural environment. A child might know when to look a therapist in the eye at the table, especially with prompts and a reward, but still not know what to do in a social situation.
The aversive training components of the therapy also drew criticism. Many found the idea of punishing children for ‘bad’ behavior such as hand-flapping and vocal outbursts hard to stomach.
Over the years, ABA has become more of a touchstone — an approach based on breaking down a skill and reinforcing through reward, that is applied more flexibly. It’s a broad umbrella that covers many different styles of therapy.
Among the many variations now in practice include pivotal response training, a play-based interactive model that sidesteps the one-behavior-at-a-time practice of traditional ABA to target what research shows to be ‘pivotal’ areas of a child’s development, such as motivation, self-management and social initiations. Another is the Early Start Denver Model (ESDM), a play-based therapy focused on children between the ages 1 and 4 that takes place in a more natural environment — a play mat, for example, rather than the standard therapist-across-from-child setup. These innovations have in part stemmed from the trend toward earlier diagnosis and the need for a therapy that could be applied to young children.
Each type of ABA is often packaged with other treatments, such as speech or occupational therapy, so that no two children’s programs may look alike. “It’s like a Chinese buffet,” says Fred Volkmar, Irving B. Harris Professor of Child Psychiatry, Pediatrics and Psychology at the Yale University Child Study Center and lead author of “Evidence-Based Practices and Treatments for Children with Autism,” a book many consider the go-to reference for ABA.
As a result, when asked whether ABA works, many experts respond: “It depends on the individual child.”
Today, Lovaas is viewed with the same kind of respectful ambivalence afforded Sigmund Freud. He’s credited with shifting the paradigm from hopeless to treatable. “Lovaas, may he rest in peace, was really on the forefront; 30 years ago, he said we can treat kids with autism and make a difference,” says Susan Levy, a member of the Center for Autism Research at the Children’s Hospital of Philadelphia. Without his passion, says Levy, many generations of children with autism might have been institutionalized. “He has to get credit for going out on a limb and saying we can make a difference.”
Testing ABA:
Given the diversity of treatments, it’s hard to get a handle on the evidence base of ABA. There is no one study that proves it works. It’s difficult to enroll children with autism in a study to test a new therapy, and especially to enroll them in control groups. Most parents are eager to begin treating their children with the therapy that is the standard of care.
There is a large body of research on ABA, but few studies meet the gold standard of the randomized trial. In fact, the first randomized trial of any version of ABA after Lovaas’ 1987 paper wasn’t published until 2010. It found that toddlers who received ESDM therapy for 20 hours a week over a two-year period made significant gains over those who got the usual care available in the community.
That year, a report from the U.S. Department of Education’s What Works Clearinghouse, a source of scientific evidence for education practices, found that of 58 studies on Lovaas’ ABA model, only 1 met its standards, and another met them only with reservations.
Those two studies found that Lovaas-style ABA leads to small improvements in cognitive development, communication and language competencies, social-emotional development, behavior and functional abilities. Neither of the high-standard studies evaluated children in literacy, math competency or physical well-being.
The following year, the U.S. Agency for Healthcare Research and Quality commissioned a stringent review of studies on therapies for children with autism spectrum disorders, with similar results. Of 159 studies, it deemed only 13 to be of good quality; for ABA-style therapies, the review focused on two-year, 20-hour-a-week interventions.
The review concluded that early intensive behavioral and developmental therapies, including the Lovaas model and ESDM, are effective for improving cognitive performance, language skills and adaptive behavior in some children. The results for intensive intervention with ESDM in children under the age of 2 were “preliminary but promising.” There was little evidence to assess other behavioral therapies, the review’s authors wrote, and information was lacking on what factors might influence effectiveness and whether improvements could carry over outside of the treatment setting.
Levy, who served on the review’s expert panel, says although the evidence in favor of ABA is not all of the highest quality, the consensus in the field is that ABA-based therapy works.
“There is a lot of good clinical evidence that it is effective in helping little kids learn new skills and can appropriately intervene with behaviors or characteristics that may interfere with progress,” says Levy. There are also other types of ABA that might be more appropriate for older children who need less support, she says.
Broadly speaking, the body of research over the past 30 years supports the use of ABA, agrees Volkmar. “It works especially well with more classically challenged kids,” Volkmar says — those who may not be able to speak or function on their own. These are, however, exactly the people that anti-ABA activists say need protection from the therapy.
Most experts acknowledge that there is a segment of children for whom ABA might be less appropriate — say, those who don’t need much support. One active area of research is scanning the brains of children to try to understand who responds and why. “Probably, as we go further down this path, we’ll see kids whose brains don’t change in response to treatment. They’re going to emerge as an important group,” says Volkmar. “We don’t know enough about them.”
Being able to identify those children who don’t have the expected neurological response — or being able to classify those who do into meaningful groups — might make it possible to fine-tune therapy.
“One day, it would be nice to match the treatment approach based on more information from these profiles rather than one-model-fits-all treatment,” says Karen Pierce, co-director of the Autism Center of Excellence at the University of California, San Diego, who uses imaging to study people with autism. “If we’re more informed, the treatment will be more successful.”
The pushback:
In December 2007, a series of signs in the style of ransom notes started appearing around New York City. One read, in part, “We have your son. We will make sure he will not be able to care for himself or interact socially as long as he lives.” It was signed “Autism.” The sign and others were part of a provocative ad campaign by New York University’s Child Study Center.
The campaign unintentionally provoked an onslaught of criticism and rage from some advocacy groups against the center, which offers ABA. Many of the vocal activists once received ABA, and they reject both the therapy’s methods and its goals.
Ne’eman, then a college student, was at the forefront of the pushback. One major criticism of ABA: the continued use of aversive therapy including pain, such as electric shock, to deter behaviors such as self-injury. Ne’eman cites a 2008 survey of leaders and scholars in the field of ‘positive behavior interventions’ — ABA techniques that emphasize desirable behaviors instead of punishing disruptive ones. Even among these experts, more than one-quarter regarded electric shock as sometimes acceptable, and more than one-third said they would consider using sensory punishment — bad smells, foul-tasting substances or loud or harsh sounds, for example. Ne’eman calls these numbers “disturbing.”
He and others also reject what they say was Lovaas’ underlying goal: to make children with autism ‘normal.’ Ne’eman says that agenda is still alive and well among ABA therapists, often encouraged by parents who want their children to fit into society. But, “those aren’t necessarily consistent with the goals people have for themselves,” he says.
The core problem with ABA is that “the focus is placed on changing behaviors to make an autistic child appear non-autistic, instead of trying to figure out why an individual is exhibiting a certain behavior,” says Reid, a young man with autism who had the therapy between ages 2 and age 5. (Because of the controversial nature of ABA and to protect his privacy, he asked that his full name not be used.) The therapy was effective for Reid. In fact, it worked so well that he was mainstreamed into kindergarten without being told he had once had the diagnosis. But he was bullied and picked on in school, and always felt different from the other children for reasons he didn’t understand, until he learned in his early teens about his diagnosis. He had been taught to be ashamed of his repetitive behaviors by his therapists, and later by his parents, who he assumes just followed the experts’ advice. He never realized these were signs of his autism.
Reid says he worries ABA forces children with autism to hide their true nature in order to fit in. “It’s taken me a long time to not be ashamed of being autistic, and that only came because I got the chance to learn from other autistic people to be proud of who I am,” he says.
“There is a lot of good clinical evidence that it is effective in helping little kids learn new skills.” Susan Levy
The middle ground:
There might be middle ground between critics and supporters of ABA, says John Elder Robison, bestselling author of “Look Me In The Eye,” who was diagnosed with Asperger syndrome at age 40.
Because of his late diagnosis, Robison did not receive ABA himself, but he has become involved in the issue on behalf of those who did. He envisions a place for ABA for people with autism — as long as it’s done well. That means a focus on teaching skills, rather than efforts toward normalization or suppressing autism-related behaviors: helping a child who could not communicate begin to talk and engage with other kids at school, for instance. “That is life-changing in a good way,” he says. Ditto an ABA therapist who helps a high school or college student become more organized. The emphasis should be on learning to function in areas the individual chooses, not on changing who she is, Robison says.
This approach will require oversight from people with autism, says Robison. “ABA programs and practitioners are going to need to accept guidance from adult versions of people they propose to treat,” he says. “What was not clear in the past is that we are the clients; we [should] have a say in what happens.”
Advocates say scientists also need to be open to the fact that ABA might not work for all. There is increasing evidence, for example, that children with apraxia, or motor planning difficulties, can sometimes understand instructions or a request, but may not be able to mentally plan a physical response to a verbal request.
Ido Kedar, who at 16 published his own memoir, “Ido in Autismland: Climbing out of Autism’s Silent Prison” writes on his blog that he spent the first half of his life “completely trapped in silence.” Kedar received 40 hours a week of traditional ABA therapy, in addition to speech therapy, occupational therapy and music therapy. But he still could not speak, communicate nonverbally, follow instructions or control his behavior when asked, for instance, to pick up the correct number of sticks. Kedar understood the request, but was unable to coordinate his knowledge with his physical movement. He was humiliated when the ABA therapist reported that he had “no number sense.”
Many researchers who study ABA welcome input of voices like Kedar’s. “I feel like it is the most wonderful, amazing thing to be able to talk with adults with autism about their experiences,” says Annette Estes, professor of speech and hearing sciences at the University of Washington in Seattle. “We all have a lot to learn from each other.” Estes led two studies of ESDM for children with early signs of autism. She says the worst stories she has heard are not from people who had traumatizing therapy, but from those who got no therapy at all.
“They have horrible memories of being bullied at school and [having] no one to help them or include them or help them make friends or handle tricky social situations,” she says. “I get letters from people begging us to expand services to adults to help them learn how to date and be less lonely and isolated.”
There is not likely to be an easy end to this discussion, and in the meantime, parents must do the best they can. Quinones-Fontanez says she understands the anti-ABA argument, but she wonders how much the perspective of those who don’t need a lot of support applies to her son. ABA, she says, works for him: “I don’t find it to be abusive.”
“I am his advocate, and I will advocate for him because he’s not able to do that for himself,” she says. “I try to understand him as best I can.”
Cite this article: https://doi.org/10.53053/RLLL6075